Balancing the brain: GABA receptors in mood and cognition
In patients with anxiety, depression, and other mood disorders, GABA signalling - the brain’s main inhibitory system - is often disrupted. Dr Elif Engin, Assistant Professor of Psychiatry and Associate Neuroscientist at Harvard University, studies GABA-A receptors to understand the neural mechanisms underlying these conditions.
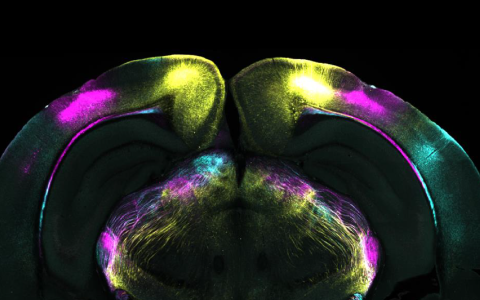
Dr Engin’s current research focuses on specific GABA-A receptor subtypes, particularly those containing the α5 subunit. The α5 subunit is uniquely concentrated in the hippocampus and likely has a role to play in memory and learning.
In a recent SWC Seminar, she presented her research, and in this Q&A, she discusses her work in mood and anxiety disorders.
What first got you interested in the brain, and specifically GABA receptors?
I was really interested in psychology, psychiatry and mental health in general. It became very clear, very quickly, that you can't understand any of those things without understanding the brain.
When I first got into the field, probably like many other students, I had these completely unrealistic, very high goals. Like, we're just going to understand how the brain works, and then we will know how depression happens.
My interest in GABA receptors came over time as I started to work more on the mechanisms of things like anxiety.
I work on animals, and while we can't really model anxiety or depression in the human sense, we can model some components of those things. GABA receptors are very intensely involved in all of those processes. There are already a number of drugs that target GABA receptors that have been used in therapeutics for over half a century now.
I went from ‘I’ll solve mental illness problems’ to ‘I'll try to understand this little component’.
What questions are you focused on now in your research?
In recent years, most of our research has focused on early development and the effects of early developmental experiences on the development of the GABA system. We then study the consequences of that for long-term changes in behaviour.
We are trying to get to the question of how things like early life trauma or early life exposure to drugs lead to susceptibility to psychiatric illness. And, is the GABA system a mediator in this equation?
What are the developmental windows where effects on these systems have long-lasting consequences?
What got me interested in early developmental experiences is that GABA-A receptors go through a lot of developmental changes after birth.
In rodents, a lot of the things that happen postnatally, in terms of brain development, happen prenatally for humans. But for GABA-A receptor changes, there are also postnatal changes in humans within the first few years of life.
The question became, while there is this developmental plasticity in the GABA system, what happens if you have an insult to the system? What happens to all that plasticity and all those changes - do some of the disruptions become permanent over time?
What have you found so far?
So far, it seems complicated, as many things are. But we have found certain behavioural deficits that correspond with certain permanent-looking changes in the expression of GABA receptors in the hippocampus, and the two seem to be linked.
Now we're trying to confirm if that is a causal link. We're trying to go step by step what's happening at the receptor level. What does that lead to at the cellular level? How does that affect things at the network level? And then how does that translate to the behaviour of the whole animal?
Could you tell us more about your work on the α5-containing GABA-A receptors in the hippocampus?
These receptors mediate tonic inhibition, that is, low-level background inhibition, controlling neuronal excitability. We have shown that mice lacking α5 receptors in a specific area of the hippocampus – the dentate gyrus - showed normal performance on simple tasks but struggled with complex memory tasks requiring pattern separation.
This indicates that α5 receptors help distinguish similar experiences. Recordings revealed more, but less precise, sharp-wave ripples, suggesting that α5 receptors refine when and where memory replay occurs.
We’ve found that the receptors also move between synaptic and extrasynaptic sites depending on activity, highlighting their dynamic role in maintaining memories.
Our findings underscore the need for a more nuanced approach to the development of α5-targeting drugs as cognitive enhancers.
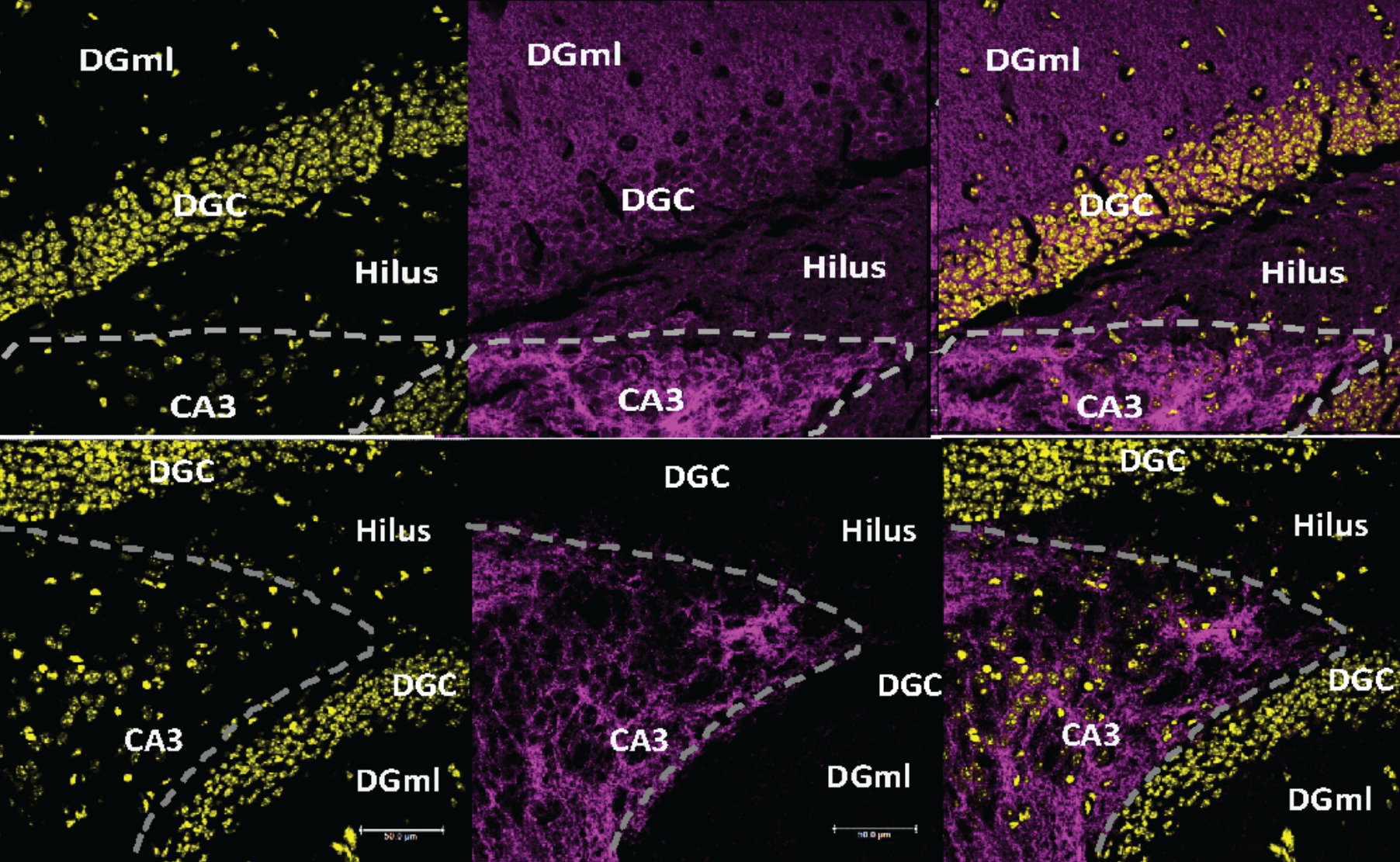
Immunofluorescence staining of coronal sections of mouse brain showing α5 in purple. The bottom row show mouse brain lacking α5 receptors in the dentate gyrus.
How close do you think we are to cell-type-specific or circuit-specific GABA interventions – whether as cognitive enhancers or treatments for mood disorders?
I don't know if it's going to be implemented in humans, but we have ways of manipulating circuits specifically. So that part might be fairly close.
But I am not sure if we are able to translate what we have learned from computational and animal models to humans, and especially to psychiatric patients.
As researchers, we usually take a reductionist approach and try to make the questions as simple as possible. But then, when you're faced with a psychiatric patient, even the diagnoses lose meaning. They feel artificial because there is just so much complexity in a person. What we learn from simplified experimentation is really difficult to apply clinically.
How do you balance your research with your clinical practice?
The clinical practice is quite recent. I have always been very interested in mental health. The idea of having a more direct impact on the lives of people who suffer from these disorders sounded really attractive. Just as I was starting as a clinician, I received funding for my research, and I decided to keep going with both for as long as possible.
I'm at the best place for this because McLean Hospital has a very long tradition of combining research and clinical work. We have a small but mighty group of neuroscientists who try to study psychiatrically relevant questions using basic and translational neuroscience approaches.
But it is tough. My research is very fundamental. I’m hoping that as I mature in this dual role, I will find ways of bringing a new perspective to either area, but so far I'm living two completely separate lives.
What do you hope your work will change about how we understand mental illness?
I think that α5 has a lot of potential as a therapeutic target, as indicated by some of my early work, as well as our more recent studies. I think, combined with the work of some other groups, it may be that we can convince everyone that α5 is actually a viable target for things like depression.
For a long time, we have had the serotonin hypothesis of depression – that it happens because people don't have enough serotonin. But this ignores the fact that when you give someone a drug to increase serotonin levels, these increase within two hours - but it takes them a whole month of taking this drug to actually get antidepressant effects.
We're now coming to the understanding that depression is linked to neuroplasticity. α5 has great potential to be a drug target, and something that people can take once and continue to have the benefits even if they're not taking something every day. And it has a lot of potential to be a drug relatively free of side effects – something that is a big issue for most current treatments for mental health.
I hope that over time, our work will contribute to more specific therapies for different disorders.
What's the next piece of the puzzle for your research?
So we have been really focused on this early developmental effects piece. This is part of the idea that early life stress is closely linked to later susceptibility to mental illness.
We're trying to figure out if a permanent change in α5 expression and function that results from early life stress might be part of that.

Biography
Dr. Elif Engin is a clinician-scientist whose work bridges neuroscience research with clinical practice as a therapist. She completed her PhD in Behavioral Neuroscience at the University of Alberta in Canada, followed by postdoctoral training in the laboratory of Dr. Uwe Rudolph at Harvard Medical School, where she focused on the genetic neuropharmacology of GABAA receptors. Since 2017, Dr. Engin has served as an Assistant Professor of Psychiatry at Harvard Medical School and a principal investigator at McLean Hospital. Her laboratory investigates how early developmental experiences, particularly early life stress, influence the maturation of the brain’s GABAergic system, with a specific focus on the hippocampus. By exploring the molecular and cellular mechanisms underlying vulnerability to psychiatric disorders, Dr. Engin’s work aims to identify novel targets for therapeutic intervention. In addition to her research, Dr. Engin holds a degree in Clinical Mental Health Counseling and is a practicing clinician at the OCD Institute at McLean Hospital. She is the recipient of several awards, including the Alfred Pope Young Investigator Award and the Brain and Behavior Research Foundation Young Investigator Award.