Towards a mechanistic understanding of psychosis
Interview with Dr Katharina Schmack, Group Leader at Francis Crick Institute and University College London, conducted by April Cashin-Garbutt
Although we all live in the same physical world, we each have a unique subjective experience. This subjectivity makes it challenging to study psychosis, when people experience a loss of contact with reality. In a recent SWC Virtual Seminar, Dr Katharina Schmack discussed her research exploring hallucination-like perceptions in humans and mice. In this Q&A, she elaborates on why it has traditionally been difficult to study disturbances in perception and her drive to find mechanistic treatment targets for psychotic disorders.
How is psychosis characterised and why have perception disturbances traditionally been difficult to study biologically?
Psychosis is a state of altered contact with reality. It is the hallmark of many severe brain disorders, including schizophrenia, and is characterised by altered perceptions and thoughts such as hallucinations and delusions.
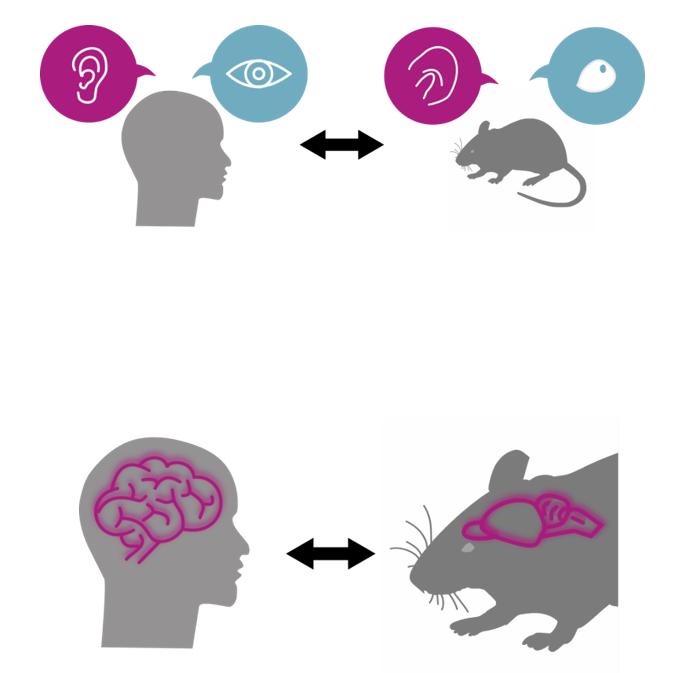
Perception disturbances are subjective in nature. This poses challenges to studying psychosis in humans but also in model organisms like mice, which typically allow us to dig deep into the biology by providing access to tools and manipulations.
How did you overcome this problem?
We developed a framework that uses behavioural tests and computational modelling to measure psychosis-like experiences in mice. The mice play something like a computer game where we present them with tones and they have to tell us when they hear tones.
We can also measure how confident the mice are in hearing these tones. Sometimes they report hearing tones even when we do not present them with tones, and do so with high confidence. That is what we call ‘hallucination-like’ or ‘psychosis-like’ perception and it is how we engage some of the mechanisms that we think are also implicated in hallucinations. We can then study these mechanisms.
How did you use this model of hallucinations and what were your key findings?
We looked at the role of dopamine, which is a neurotransmitter that has previously been shown to be involved in psychosis. It has been thought for a long time that too much dopamine induces these symptoms/experiences of psychosis, hallucinations, and delusions. What has not been clear is how exactly dopamine leads to these experiences.
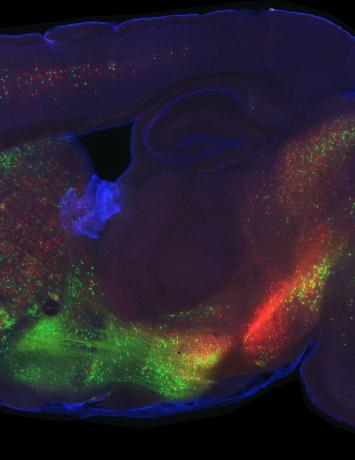
We used these hallucination-like perceptions by having mice play this computer game, while we also measured dopamine in the brain. What we found was that too much dopamine leads to hallucination-like perceptions. We were able to use some computational models to show that dopamine seems to code for expectations.
What we think is happening is that when there is too much dopamine, there is an imbalance between how current sensory input is integrated with current expectation. Perception becomes sculpted more strongly by our expectations and one starts to hear what they are expecting leading to the emergence of hallucinations.
In line with this we found when we actively increased dopamine in the brains of mice, they have more of these hallucination-like perceptions. If we block dopamine with an antipsychotic drug, they stopped having these hallucination-like perceptions. This is how we determined causation.
The exciting thing about this is that the idea that too much dopamine leads to hallucinations has been around for a long time, but now we can provide some insights into how this might happen and unfold at the level of processing in the brain.
What is the next piece of the puzzle your research is going to focus on?
One thing we are really interested in is how dopamine is controlled in the brain, and identifying these mechanisms to then develop better treatments. Most treatments already target dopamine, but they don’t do this in a good way. At the moment, treatments mainly block dopamine receptors, thereby blocking transmission of the signal, but what seems to be happening in psychosis is that there is too much dopamine there in the first place.
This blocking of the receptors has some side effects – people don’t really like taking these drugs and they also have the effect that when people stop taking these drugs, they get what we call rebound psychosis, which are really bad psychotic outbreaks.
One way to overcome this is to try to modulate endogenous mechanisms by which the brain controls dopamine release. We need to see whether we can target the underlying abnormality, which is too much dopamine. We plan to look at other neurons in the brain that control dopamine release and see whether they play a role in psychosis-like behaviour, and see whether we can manipulate them in a way that could be used for new therapies.
Will this research help to identify new biological targets for the treatment of schizophrenia? How close do you think we are to this?
Essentially our driving motivation is to develop new treatments. One important thing to bear in mind is that, as of now, we don’t have any mechanistic treatments. All the treatments we have were discovered by serendipity.
The hope is to gain some mechanistic understanding that can then be used for new treatments. We first need to do some basic research and understand what is going on, then I hope that we can go to new treatments in a straightforward way. But it’s important to understand the mechanisms, not blindly test some treatments.

About Dr Katharina Schmack
Katharina Schmack received her MD/PhD equivalent from Charité, Berlin in 2009. She then completed her postdoctoral training, clinical scientist fellowship and psychiatry specialization at Charité, Berlin. In 2018, she was awarded a research fellowship from the German National Academy of Sciences, Leopoldina, and joined Cold Spring Harbor Laboratory, New York, as a research investigator in Adam Kepecs’ group. In September 2021, she opened her own lab at the Francis Crick Institute, London. As a Clinical Group Leader, her appointment is shared with the UCL – Division of Psychiatry, and she splits her time between research and patient care.
Her research focuses on psychosis. Her group investigates the neural circuits and immune processes giving rise to hallucinations and other psychotic symptoms. Using a cross-species approach, they study both patients and mice with behavioural tests, computational models, and in-vivo measures and manipulations.